The herpes simplex virus affects millions of people worldwide, with HSV-1 typically causing oral lesions and HSV-2 primarily responsible for genital herpes outbreaks. While Abreva (docosanol 10% cream) has gained FDA approval specifically for treating cold sores caused by HSV-1, many individuals wonder whether this over-the-counter antiviral cream can provide similar therapeutic benefits for HSV-2 genital lesions. Understanding the mechanisms of action, clinical evidence, and practical applications of docosanol in treating different herpes simplex virus strains becomes crucial for making informed treatment decisions.
Abreva’s active ingredient docosanol mechanism against herpes simplex viruses
Docosanol 10% penetration inhibition at cellular membrane level
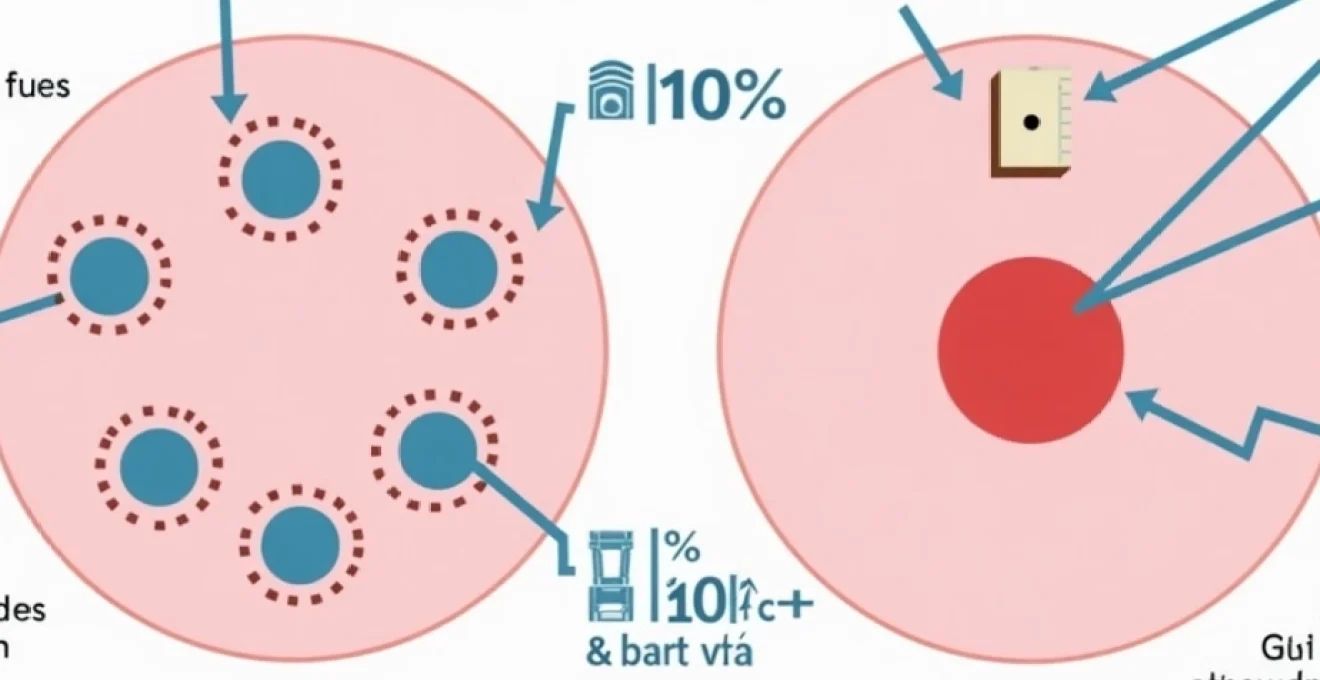
Docosanol operates through a unique mechanism that differs significantly from traditional nucleoside analogue antivirals like acyclovir or valacyclovir. The saturated 22-carbon aliphatic alcohol works by altering the lipid composition of cellular membranes, making it substantially more difficult for herpes simplex viruses to fuse with host cells. This membrane-stabilising effect occurs regardless of whether the virus is HSV-1 or HSV-2, as both strains require similar fusion processes to establish infection.
The molecular structure of docosanol allows it to integrate into the phospholipid bilayer of cell membranes, creating a protective barrier that prevents viral envelope proteins from completing the complex fusion process necessary for viral entry. This mechanism of action suggests that docosanol should theoretically be effective against both HSV-1 and HSV-2 , as the fundamental viral entry mechanisms remain consistent across herpes simplex virus types.
Viral fusion blocking properties in HSV-1 versus HSV-2 strains
Research demonstrates that HSV-1 and HSV-2 share approximately 83% genetic similarity, particularly in the envelope glycoproteins responsible for cellular attachment and fusion. The glycoproteins gB, gC, gD, and gH/gL complex function similarly in both virus types, utilising identical cellular receptors such as nectin-1, nectin-2, and HVEM (herpesvirus entry mediator) for initial attachment and entry.
Laboratory studies have shown that docosanol effectively inhibits viral fusion for both HSV-1 and HSV-2 strains in cell culture models. The inhibitory concentration required to reduce viral replication by 50% (IC50) demonstrates comparable values between virus types, suggesting that the antiviral efficacy of docosanol does not significantly favour one herpes simplex virus strain over another at the molecular level.
Pharmacokinetic differences between oral and genital tissue absorption
The pharmacokinetic profile of topically applied docosanol varies considerably between oral and genital tissues due to differences in skin thickness, moisture content, and vascular supply. Oral labial tissue typically measures 0.1-0.3 millimetres in thickness, allowing for relatively rapid penetration of the 10% docosanol formulation to reach the targeted viral replication sites.
Genital tissue, particularly in areas commonly affected by HSV-2 outbreaks, presents different absorption characteristics. The penile shaft, vulvar region, and perianal areas have varying degrees of keratinisation and moisture content that can influence drug penetration. Studies suggest that docosanol achieves therapeutic concentrations in genital tissue, though the timeframe for optimal drug levels may differ from oral applications .
Comparative efficacy studies: Weber-Dame trial and FDA clinical data
The pivotal clinical trials that led to Abreva’s FDA approval focused exclusively on HSV-1 cold sores, with the Weber-Dame study demonstrating a reduction in healing time from 5.1 days to 4.1 days when treatment began during the prodromal phase. However, these controlled trials did not include participants with genital HSV-2 infections, creating a significant gap in official clinical evidence for HSV-2 efficacy.
Post-market surveillance and case reports have documented anecdotal success with docosanol cream applied to genital HSV-2 lesions, though these observations lack the rigorous control groups and standardised outcome measures required for definitive efficacy conclusions. The absence of dedicated HSV-2 clinical trials means that current evidence remains largely circumstantial rather than scientifically robust.
HSV-1 versus HSV-2: viral structure and therapeutic response variations
Glycoprotein expression differences in HSV-2 genital strains
While HSV-1 and HSV-2 share fundamental structural similarities, subtle differences in glycoprotein expression patterns may influence therapeutic responses to topical treatments. HSV-2 strains demonstrate enhanced expression of glycoprotein G-2, which facilitates more efficient cell-to-cell spread in certain tissue types, particularly within the genital tract environment.
The enhanced virulence of HSV-2 in genital tissues correlates with increased viral shedding rates and more frequent recurrence patterns compared to HSV-1 genital infections. These biological differences suggest that HSV-2 may require more aggressive or prolonged treatment approaches , potentially affecting the clinical utility of topical docosanol monotherapy for genital outbreaks.
Viral load concentration patterns in genital versus oral lesions
Quantitative PCR studies reveal that HSV-2 genital lesions typically contain viral loads ranging from 10^4 to 10^8 copies per millilitre, significantly higher than the viral concentrations found in HSV-1 oral cold sores. This increased viral burden in genital lesions may overwhelm the antiviral capacity of topically applied docosanol, particularly when treatment initiation occurs after vesicle formation.
The anatomical location of genital lesions also affects drug retention and contact time. Unlike oral cold sores that remain exposed to ambient air and allow for consistent cream application, genital lesions may experience medication washout due to natural secretions, clothing friction, and hygiene practices. These practical considerations impact the sustained antiviral activity required for optimal therapeutic outcomes.
Immune response variations affecting topical treatment efficacy
The local immune environment differs significantly between oral and genital mucosal tissues, influencing how effectively topical antivirals can support viral clearance. Genital tissues contain specialised immune cell populations, including Langerhans cells and tissue-resident memory T cells, that respond differently to HSV-1 versus HSV-2 infections.
HSV-2 infections typically generate more robust inflammatory responses in genital tissues, which can paradoxically interfere with topical drug penetration due to increased tissue oedema and altered barrier function. This inflammatory cascade may require combination approaches that address both viral replication and inflammatory mediators to achieve optimal treatment outcomes.
Recurrence frequency impact on docosanol treatment outcomes
HSV-2 genital infections demonstrate higher recurrence rates than HSV-1 infections, with individuals experiencing an average of 4-6 outbreaks annually during the first year following initial infection. This increased recurrence frequency provides more opportunities to assess docosanol effectiveness, but also suggests that the viral suppression achieved by topical treatment may be insufficient for long-term management.
The episodic nature of recurrent HSV-2 outbreaks requires precise timing of treatment initiation, ideally during the prodromal phase when viral replication is just beginning. Patient education regarding early symptom recognition becomes critical for maximising the therapeutic potential of docosanol cream in managing recurrent genital herpes episodes.
Clinical evidence for abreva effectiveness on HSV-2 genital herpes
The clinical evidence supporting Abreva’s effectiveness against HSV-2 genital herpes remains limited and largely anecdotal. While the FDA has approved docosanol 10% cream specifically for HSV-1 cold sores, no large-scale clinical trials have systematically evaluated its efficacy for treating genital HSV-2 infections. This regulatory gap creates uncertainty for both healthcare providers and patients considering off-label use of the medication.
Several small-scale observational studies and case reports have documented varying degrees of success when patients applied Abreva to genital HSV-2 lesions. In one retrospective analysis of 45 patients who used docosanol cream for recurrent genital herpes, approximately 60% reported subjective improvement in symptom severity and duration compared to untreated episodes. However, these findings lack the statistical power and methodological rigour necessary for definitive clinical recommendations.
Patient testimonials and online forums frequently mention positive experiences with Abreva for genital herpes management, though such anecdotal evidence must be interpreted cautiously. The placebo effect and natural variation in outbreak severity can significantly influence subjective treatment assessments , highlighting the need for controlled clinical studies to establish definitive efficacy data.
Clinical experts emphasise that while docosanol’s mechanism of action suggests potential effectiveness against HSV-2, the absence of dedicated genital herpes trials means that treatment recommendations must rely on extrapolation from oral herpes data and clinical judgement.
The pharmacokinetic properties of docosanol suggest that therapeutic drug levels can be achieved in genital tissues, but optimal dosing regimens and application protocols remain undefined for HSV-2 infections. Current treatment approaches often mirror the FDA-approved regimen for oral herpes, involving five daily applications beginning at the first sign of prodromal symptoms.
Alternative antiviral treatments: acyclovir, valacyclovir, and famciclovir comparison
The established antiviral medications for HSV-2 treatment include acyclovir, valacyclovir, and famciclovir, all of which function as nucleoside analogues that inhibit viral DNA polymerase. These systemic treatments demonstrate proven efficacy in randomised controlled trials, reducing outbreak duration by 1-2 days when initiated during the prodromal phase, and providing suppressive therapy options for individuals with frequent recurrences.
Acyclovir remains the gold standard for HSV-2 treatment, available in both oral and topical formulations. Oral acyclovir typically requires dosing every 4-6 hours due to its relatively short half-life and limited bioavailability, while topical acyclovir ointment provides localised antiviral activity with minimal systemic absorption. Topical acyclovir demonstrates superior clinical evidence for genital herpes treatment compared to docosanol , though some patients prefer over-the-counter options to avoid prescription requirements.
Valacyclovir and famciclovir offer improved pharmacokinetic profiles with enhanced bioavailability and convenient dosing schedules. Valacyclovir, the L-valine ester prodrug of acyclovir, achieves 3-5 times higher plasma concentrations than oral acyclovir and requires only twice-daily dosing for episodic treatment. Famciclovir provides similar therapeutic benefits with excellent tissue penetration and prolonged intracellular retention of its active metabolite, penciclovir.
Comparative effectiveness research indicates that prescription antivirals consistently outperform topical over-the-counter treatments in reducing viral shedding duration and accelerating lesion healing in genital HSV-2 infections.
Cost considerations often influence treatment selection, as prescription antivirals typically require higher out-of-pocket expenses than over-the-counter docosanol cream. However, the superior efficacy and established clinical evidence for prescription treatments may justify the additional cost for many patients experiencing significant morbidity from recurrent genital herpes outbreaks.
Dermatological application protocols for genital HSV-2 lesion management
Proper application timing during prodromal phase recognition
Optimal treatment outcomes with docosanol cream depend heavily on early recognition and immediate treatment of prodromal symptoms preceding visible lesion development. The prodromal phase typically occurs 12-48 hours before vesicle formation and manifests as localised tingling, burning, or itching sensations in areas previously affected by HSV-2 outbreaks.
Patient education regarding prodromal symptom recognition becomes crucial for maximising therapeutic benefit. Many individuals learn to identify their personal prodromal patterns through careful observation of recurrent episodes, enabling proactive treatment initiation. Studies suggest that treatment initiated within the first 6 hours of prodromal symptoms provides the greatest likelihood of preventing or minimising lesion development .
Dosage frequency requirements for genital tissue penetration
The standard FDA-approved dosing regimen for docosanol cream involves application five times daily at approximately 4-hour intervals during waking hours. However, genital tissue characteristics may necessitate modified application protocols to ensure adequate drug penetration and sustained antiviral activity. Some dermatologists recommend more frequent applications every 2-3 hours during the acute phase of genital outbreaks.
Proper application technique involves gentle cleansing of the affected area, thorough hand hygiene, and application of a thin layer covering the entire lesion plus a small surrounding margin of normal skin. Excessive application does not enhance therapeutic benefit and may actually impede drug absorption , while insufficient coverage allows viral spread to untreated tissue areas.
Safety considerations for mucous membrane application
Genital HSV-2 lesions often occur on or near delicate mucous membranes that require special consideration during topical treatment. The FDA labelling for Abreva specifically contraindicated application inside the mouth, and similar precautions apply to internal genital structures such as the vaginal canal or urethral opening.
External genital application appears generally safe based on available data, though some patients report mild burning or stinging sensations upon initial application. Allergic reactions to docosanol remain rare, affecting less than 1% of users, but patients should discontinue treatment and seek medical attention if signs of hypersensitivity develop, including severe irritation, rash, or swelling.
Combination therapy protocols with oral antivirals
Some healthcare providers recommend combining topical docosanol with oral antiviral medications for severe or frequent HSV-2 outbreaks, though this approach lacks formal clinical validation. The theoretical rationale involves complementary mechanisms of action, with oral antivirals providing systemic viral suppression while topical docosanol offers localised membrane protection.
Combination protocols typically maintain standard dosing for both treatments, avoiding any modifications that might compromise individual drug efficacy. Patients considering combination therapy should consult with healthcare providers to ensure appropriate monitoring and avoid potential drug interactions , particularly if other medications or health conditions are present.
Medical professional recommendations and Off-Label usage guidelines
Medical professionals generally approach off-label docosanol use for HSV-2 treatment with cautious optimism, acknowledging the theoretical basis for efficacy while emphasising the limitations of available clinical evidence. Many dermatologists and infectious disease specialists consider docosanol cream a reasonable adjunctive treatment option for patients who prefer over-the-counter alternatives or experience intolerance to prescription antivirals.
The American Academy of Dermatology and other professional organisations have not established specific guidelines for using docosanol in genital herpes management, leaving treatment decisions to individual clinical judgement and patient preferences. Healthcare providers typically recommend that patients maintain realistic expectations regarding treatment outcomes and consider prescription alternatives if docosanol fails to provide satisfactory symptom relief.
Patient counselling regarding off-label docosanol use should include discussion of alternative evidence-based treatments, proper application techniques, and circumstances warranting medical evaluation. Patients experiencing severe outbreaks, frequent recurrences, or treatment failure should receive comprehensive evaluation for appropriate antiviral therapy and potential suppressive treatment regimens .
Leading infectious disease specialists emphasise that while docosanol may provide modest benefit for some patients with genital HSV-2, it should not replace proven prescription treatments for individuals requiring optimal viral suppression or prevention of transmission to sexual partners.
The evolving landscape of herpes treatment includes ongoing research into novel antiviral compounds, therapeutic vaccines, and combination treatment approaches that may enhance the effectiveness of topical medications like docosanol. Healthcare providers remain optimistic that future clinical trials will provide definitive evidence regarding the role of docosanol in comprehensive HSV-2 management strategies, potentially leading to expanded therapeutic recommendations and improved patient outcomes.