Hair follicle drug testing represents one of the most comprehensive screening methods available today, capable of detecting substance use over extended periods. For individuals prescribed Suboxone as part of their medication-assisted treatment (MAT) for opioid use disorder, understanding whether this medication appears on hair follicle tests becomes crucial for employment, legal, and medical scenarios. Unlike standard urine or blood tests that offer relatively short detection windows, hair follicle analysis can reveal drug use patterns spanning months, making it particularly relevant for those seeking clarity about their prescribed buprenorphine-based therapy.
The complexity of hair follicle testing for Suboxone involves sophisticated analytical methods and specific detection protocols that differ significantly from conventional opioid screening. Most individuals taking Suboxone legitimately worry unnecessarily about routine drug tests , as standard panels rarely include buprenorphine detection capabilities. However, specialised hair follicle tests designed to identify medication-assisted treatment substances present different considerations that require careful examination.
Suboxone detection mechanisms in hair follicle drug testing
Buprenorphine and naloxone metabolite incorporation into hair shaft
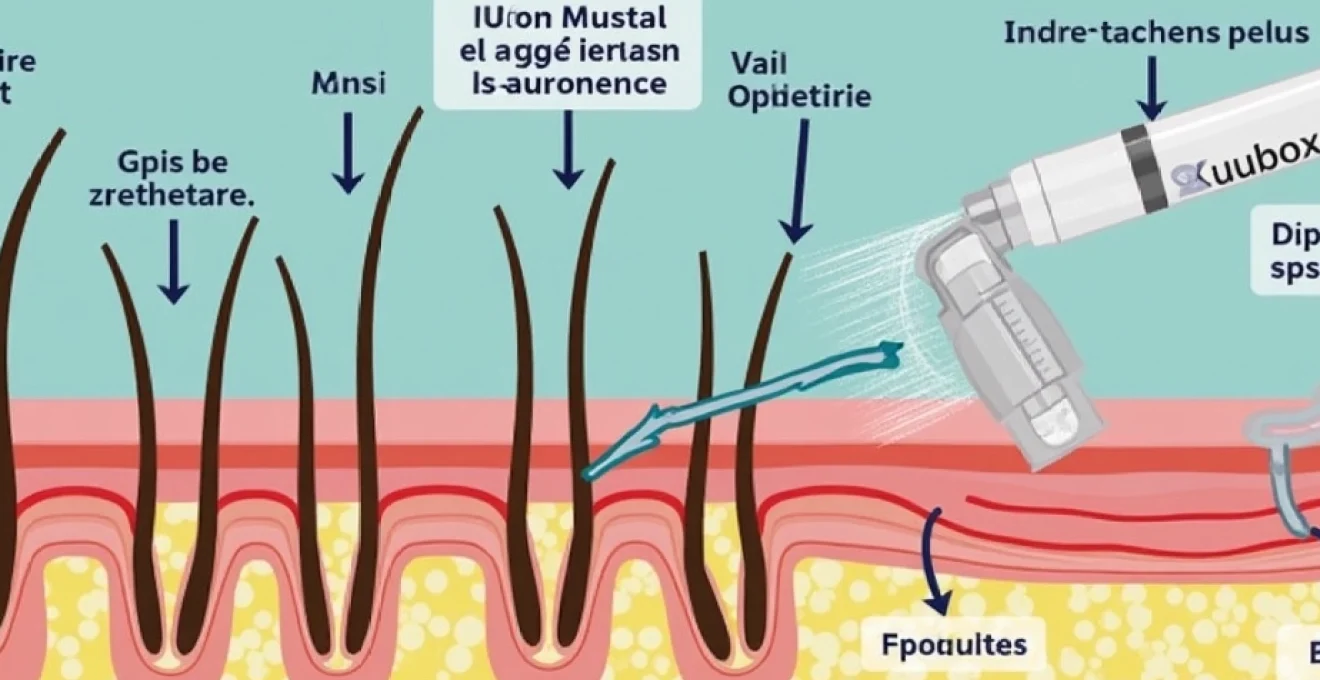
When you take Suboxone, the active compounds buprenorphine and naloxone undergo metabolic processes that create detectable markers within your hair structure. Buprenorphine metabolises into norbuprenorphine and buprenorphine-3-glucuronide , both of which can become incorporated into growing hair follicles through blood circulation. The process occurs as these metabolites travel through your bloodstream and deposit into the hair shaft during the anagen growth phase.
Naloxone, the second component of Suboxone, presents different incorporation patterns due to its rapid metabolism and shorter half-life. Laboratory analysis typically focuses on detecting nornaloxone and naloxone-3-glucuronide metabolites, though these compounds appear in significantly lower concentrations compared to buprenorphine derivatives. The detection sensitivity for naloxone metabolites in hair samples remains considerably lower than for buprenorphine, making buprenorphine the primary target for Suboxone identification in hair follicle tests.
Chronological drug deposition timeline in keratin structures
Hair growth patterns directly influence when Suboxone metabolites become detectable through follicle analysis. Your hair grows approximately 1.3 centimetres monthly, meaning substances consumed today won’t appear in testable hair samples for 7-10 days. This delay occurs because drug metabolites must travel from your bloodstream into actively growing hair cells before becoming permanently incorporated into the keratin structure.
The chronological nature of hair deposition creates a timeline that forensic analysts can potentially map to specific usage periods. Each centimetre of hair growth theoretically represents one month of potential drug exposure , allowing laboratories to segment hair samples for temporal analysis. However, this precision depends heavily on consistent growth rates, hair colour, and individual metabolic factors that can vary significantly between people.
Gas Chromatography-Mass spectrometry detection thresholds for suboxone components
Modern hair follicle testing employs GC-MS technology to identify specific Suboxone metabolites with exceptional precision. The detection threshold for buprenorphine in hair samples typically ranges from 0.5 to 2.0 nanograms per milligram of hair, depending on the analytical method employed. These sensitivity levels represent significant improvements over earlier testing technologies, enabling laboratories to detect even minimal therapeutic doses of Suboxone.
Confirmation testing protocols require dual-column analysis and spectral library matching to eliminate false positives and ensure accurate identification. The specificity of GC-MS analysis means that legitimate Suboxone use can be definitively distinguished from illicit opioid consumption , providing crucial protection for patients undergoing medication-assisted treatment programmes.
Immunoassay screening protocols for opioid replacement therapy medications
Initial screening procedures often utilise enzyme immunoassays designed to detect opioid replacement therapy medications specifically. These protocols differ substantially from standard opioid screens, requiring specialised antibodies that recognise buprenorphine and its metabolites. Many employment-related hair follicle tests do not include these specialised screening protocols , focusing instead on traditional substances of abuse.
The immunoassay screening process serves as a preliminary filter before confirmatory testing, helping laboratories identify samples requiring detailed analysis. Cross-reactivity studies demonstrate that buprenorphine immunoassays show minimal interference from other opioid medications, ensuring that your legitimate Suboxone prescription won’t trigger false positives for illicit substances.
Hair follicle testing detection windows for Buprenorphine-Based medications
90-day retrospective detection period for suboxone metabolites
The extended detection window represents both the primary advantage and concern regarding hair follicle testing for Suboxone users. Standard hair follicle analysis can potentially detect buprenorphine metabolites for up to 90 days after your last dose, significantly longer than urine testing capabilities. This extended timeframe reflects the permanent incorporation of drug metabolites into hair structure during growth phases.
However, the 90-day detection window assumes consistent hair growth and adequate hair length for testing purposes. Laboratories typically require 3.9 centimetres of hair from the crown area, representing approximately three months of growth.
The detection window may extend beyond 90 days if longer hair samples are available and analysed, potentially revealing historical Suboxone use patterns.
Understanding this extended detection period becomes particularly important when considering employment opportunities, legal proceedings, or medical evaluations where hair follicle testing might be required. Unlike urine tests that clear Suboxone metabolites within 7-10 days, hair analysis maintains detection capabilities for months after discontinuation.
Factors affecting buprenorphine concentration in hair samples
Multiple physiological and environmental factors influence the concentration of buprenorphine metabolites detected in hair samples. Hair colour significantly impacts drug incorporation rates , with darker hair typically showing higher concentrations due to increased melanin binding capacity. This phenomenon means that individuals with darker hair may test positive at lower usage levels compared to those with lighter hair colours.
Your metabolic rate, dosage frequency, and individual absorption characteristics all contribute to the final concentration detected in hair analysis. Chronic Suboxone users typically show higher metabolite concentrations compared to short-term users, though individual variation remains substantial. Chemical hair treatments, including bleaching, colouring, and straightening procedures, can reduce detectable drug concentrations by 20-80%, potentially affecting test results.
Body hair samples may be utilised when head hair is unavailable, though detection characteristics differ significantly. Body hair generally shows longer detection windows but lower metabolite concentrations compared to scalp hair, requiring adjusted analytical thresholds and interpretation protocols.
Comparison between suboxone film, tablet, and injectable formulations
Different Suboxone formulations may produce varying detection patterns in hair follicle analysis due to bioavailability and absorption differences. Sublingual films typically demonstrate consistent detection patterns due to standardised absorption rates, whilst tablet formulations may show slight variations based on dissolution characteristics. Injectable buprenorphine formulations often produce higher and more sustained hair metabolite concentrations due to their extended-release properties.
The naloxone component shows minimal variation between formulations regarding hair detection, as its rapid metabolism and low bioavailability limit incorporation into hair structure regardless of delivery method. Understanding these formulation differences becomes important when interpreting hair test results and correlating findings with prescribed treatment regimens.
Laboratory testing protocols and analytical methods
Labcorp and quest diagnostics hair follicle panel specifications
Major diagnostic laboratories employ distinct testing panels and methodologies for detecting Suboxone in hair samples. LabCorp’s comprehensive opioid panels include specific buprenorphine detection capabilities, utilising LC-MS/MS confirmation methods with detection thresholds of 0.5 ng/mg. Their testing protocols incorporate both screening and confirmation phases to ensure analytical accuracy and minimise false results.
Quest Diagnostics employs similar methodologies with slightly different threshold parameters, typically using 1.0 ng/mg cutoff levels for buprenorphine detection. Both laboratories require specific test orders for buprenorphine analysis , as standard hair follicle panels typically exclude medication-assisted treatment substances. This requirement means that routine employment or legal testing may not detect your prescribed Suboxone unless specifically requested.
The analytical turnaround time for specialised buprenorphine hair analysis typically ranges from 3-5 business days, longer than standard drug panels due to the complex confirmation procedures required. Understanding these laboratory specifications helps you anticipate testing outcomes and prepare appropriate documentation when required.
Enzyme-linked immunosorbent assay (ELISA) confirmation procedures
ELISA-based confirmation protocols provide additional analytical verification for positive buprenorphine screening results. These procedures utilise specific antibodies designed to recognise buprenorphine metabolites whilst minimising cross-reactivity with other compounds. The ELISA confirmation process typically requires 24-48 hours beyond initial screening , ensuring thorough analytical verification before reporting results.
Quality control measures within ELISA protocols include positive and negative controls, calibration standards, and proficiency testing to maintain analytical reliability. The enzyme-based detection system provides quantitative results, enabling laboratories to determine approximate usage levels and patterns based on metabolite concentrations detected.
Liquid Chromatography-Tandem mass spectrometry (LC-MS/MS) quantification
LC-MS/MS represents the gold standard for definitive Suboxone detection in hair samples, providing unparalleled specificity and sensitivity. This analytical method can distinguish between buprenorphine, norbuprenorphine, and other metabolites whilst eliminating interference from structurally similar compounds. The quantitative capabilities of LC-MS/MS enable precise measurement of drug concentrations , supporting interpretation of usage patterns and therapeutic compliance.
The triple-quadrupole mass spectrometry system used in LC-MS/MS analysis can detect buprenorphine at concentrations as low as 0.1 ng/mg, significantly below therapeutic detection thresholds. This sensitivity ensures that even minimal Suboxone exposure can be identified and quantified accurately, providing definitive confirmation of medication use.
Analytical validation procedures for LC-MS/MS include linearity studies, precision assessments, and matrix effect evaluations to ensure reliable quantification across diverse hair sample types.
The robustness of LC-MS/MS analysis makes it the preferred confirmatory method for forensic and clinical applications requiring absolute certainty.
Cross-reactivity with morphine, codeine, and synthetic opioids
Understanding cross-reactivity patterns becomes crucial when interpreting hair follicle test results for individuals taking Suboxone alongside other medications. Buprenorphine shows minimal cross-reactivity with traditional opioids like morphine and codeine due to its unique chemical structure and metabolic pathway. This selectivity means that concurrent pain medication use typically won’t interfere with Suboxone detection or create false positive results.
Synthetic opioids, including fentanyl analogues and tramadol, demonstrate negligible cross-reactivity with buprenorphine-specific assays. However, some synthetic compounds may interfere with initial immunoassay screening, necessitating confirmatory testing to establish definitive identification. The analytical specificity of modern testing methods ensures that legitimate Suboxone use can be distinguished from illicit opioid consumption with confidence.
| Substance | Cross-Reactivity with Buprenorphine Assays | Interference Risk |
|---|---|---|
| Morphine | <0.1% | Minimal |
| Codeine | <0.1% | Minimal |
| Fentanyl | <0.05% | None |
| Tramadol | <0.2% | Low |
Legal and medical considerations for suboxone hair testing
The legal landscape surrounding hair follicle testing for prescribed medications presents complex considerations that vary significantly across jurisdictions and contexts. Employment-related hair testing for Suboxone occupies a particularly nuanced legal space , where discrimination laws intersect with workplace safety requirements and drug-free workplace policies. The Americans with Disabilities Act provides certain protections for individuals undergoing medication-assisted treatment, though these protections may not extend to safety-sensitive positions.
Documentation requirements for legitimate Suboxone prescription become paramount when facing hair follicle testing in legal or employment contexts. Maintaining current prescription records, treatment provider documentation, and medical necessity letters helps establish the therapeutic nature of detected buprenorphine metabolites. Proactive disclosure of prescribed Suboxone use often prevents misunderstandings and demonstrates transparency regarding medication-assisted treatment participation.
Medical review officer protocols typically accommodate prescribed medication use, requiring additional documentation and verification before reporting positive results as violations. Understanding these procedures helps individuals navigate testing requirements whilst protecting their privacy rights and treatment continuity. The confidential nature of medical information generally limits disclosure of specific prescription details beyond basic verification requirements.
Child custody proceedings and family court evaluations increasingly incorporate hair follicle testing as evidence of parental fitness and stability. Legitimate Suboxone use generally supports rather than undermines child custody interests , demonstrating commitment to recovery and responsible medical care. However, proper documentation and expert testimony may be required to distinguish therapeutic use from substance abuse patterns.
The evolving legal recognition of medication-assisted treatment as standard medical care continues to influence how courts and employers interpret positive results for prescribed buprenorphine.
Recent legislative developments in several jurisdictions explicitly protect MAT patients from discrimination, though implementation and enforcement remain inconsistent across different sectors and regions.
False positive and false negative results in buprenorphine hair analysis
False positive results for buprenorphine in hair follicle testing remain exceptionally rare due to the compound’s unique chemical structure and specific detection methods employed. The analytical selectivity of modern LC-MS/MS systems virtually eliminates the possibility of misidentification from other substances, though laboratory contamination or sample mix-ups represent potential sources of erroneous results. Quality assurance protocols within accredited laboratories typically prevent these administrative errors through chain-of-custody procedures and duplicate analysis verification.
Environmental contamination represents a theoretical concern for buprenorphine hair testing, though practical exposure scenarios remain limited due to the medication’s controlled distribution and handling requirements. Unlike some substances that can be absorbed through external contact, buprenorphine requires systemic absorption to produce detectable hair metabolite concentrations. This characteristic provides inherent protection against passive exposure claims and supports the validity of positive test results.
False negative results present more significant concerns, particularly for individuals with certain hair characteristics or chemical treatment histories. Bleached or chemically processed hair may show reduced metabolite concentrations , potentially falling below detection thresholds despite actual Suboxone use. Similarly, individuals with very light or gray hair may demonstrate lower incorporation rates, affecting detection sensitivity and reliability.
Insufficient hair length or quantity can prevent adequate analysis, necessitating alternative testing methods or sample collection sites. Body hair collection may be utilised when scalp hair is unavailable, though detection characteristics differ substantially and may require adjusted interpretation criteria. Understanding these analytical limitations helps individuals and testing authorities select appropriate testing methods and interpret results within proper scientific contexts.
Recent hair growth following treatment initiation may not contain detectable metabolites despite current Suboxone use, creating apparent false negative results during the initial weeks of therapy. This phenomenon reflects the natural delay between drug consumption and hair incorporation rather than analytical failure, emphasising the importance of considering treatment timelines when interpreting test results. Advanced analytical methods continue to improve detection sensitivity and reliability, though biological limitations regarding hair growth and metabolite incorporation remain constant factors affecting test interpretation.