Distinguishing between a herpes outbreak and a common lip pimple represents one of the most frequent diagnostic challenges encountered in dermatological practice. Both conditions manifest as raised, inflamed lesions in the perioral region, yet they stem from entirely different pathophysiological mechanisms and require distinct therapeutic approaches. The confusion between these two conditions is understandable, given their initial similar appearance, particularly during the early stages of development. However, understanding the fundamental differences between viral-induced vesicular eruptions and bacterial comedonal formations can prevent misdiagnosis and ensure appropriate treatment protocols.
The clinical significance of accurate differentiation extends beyond mere academic interest. Herpes simplex virus infections carry implications for viral transmission, whilst acne lesions present primarily cosmetic and psychological concerns without contagious risk. Moreover, the therapeutic interventions for each condition differ substantially, with antiviral medications proving ineffective against bacterial acne and comedonal treatments offering no benefit for viral replication cycles.
Understanding herpes simplex virus lesions and their clinical manifestations
Herpes simplex virus infections represent a complex interplay between viral pathogenesis and host immune responses, resulting in characteristic vesicular eruptions that follow predictable patterns of development and resolution. The clinical presentation of herpes labialis involves multiple phases, each with distinct morphological characteristics that can aid in differential diagnosis when compared to non-viral skin conditions.
HSV-1 and HSV-2 pathophysiology in perioral regions
The herpes simplex virus family encompasses two primary strains that can affect the perioral region, though HSV-1 remains the predominant cause of oral manifestations. HSV-1 traditionally associates with orofacial infections, whilst HSV-2 typically causes genital lesions, though cross-contamination can occur through oral-genital contact. Both viral strains establish latent infections within the trigeminal ganglion, creating a reservoir for recurrent outbreaks throughout the host’s lifetime.
The viral tropism for neuronal tissue explains the characteristic distribution pattern of herpes lesions, which typically appear along specific dermatomes innervated by the affected nerve pathways. This neuroanatomical predisposition results in lesions that consistently appear in similar locations during recurrent episodes, a key diagnostic feature that distinguishes herpes from randomly distributed acne lesions.
Viral replication cycle and vesicular formation process
The formation of characteristic herpes vesicles results from extensive viral replication within epidermal keratinocytes, leading to cellular destruction and fluid accumulation. Upon reactivation from the dormant state, viral particles travel along nerve axons to reach the skin surface, where they begin aggressive replication cycles. The cytopathic effects of viral multiplication cause balloon degeneration of infected cells, creating intraepidermal vesicles filled with clear, protein-rich fluid containing high concentrations of infectious viral particles.
This vesicular formation process differs fundamentally from the inflammatory mechanisms underlying acne development. Herpes vesicles represent direct viral cytotoxicity , whilst acne lesions result from bacterial proliferation within sebaceous follicles. The clear fluid content of herpes vesicles contrasts sharply with the purulent material characteristic of inflamed comedones, providing another distinguishing feature for clinical assessment.
Prodromal symptoms: tingling, burning, and neurological precursors
Perhaps the most distinctive feature of herpes outbreaks lies in the prodromal phase, during which patients experience characteristic sensory disturbances preceding visible lesion formation. These neurological symptoms result from viral reactivation and migration along sensory nerve pathways, creating sensations of tingling, burning, or sharp pain in the affected distribution area. The prodromal phase typically lasts 6-24 hours before visible lesions appear, providing a diagnostic window for early intervention.
The prodromal sensations associated with herpes reactivation represent viral movement along nerve pathways, creating distinctive neurological symptoms that precede visible lesion formation by several hours to days.
Recognition of prodromal symptoms enables early initiation of antiviral therapy, potentially preventing or minimising the subsequent outbreak’s severity. Patients familiar with their individual patterns of herpes reactivation often report identical sensory experiences preceding each recurrent episode, reinforcing the neurotropic nature of the viral infection.
Typical progression timeline from initial outbreak to crusting phase
The natural history of herpes labialis follows a predictable progression through distinct clinical phases, each with characteristic morphological features and symptomatology. The initial vesicular phase typically lasts 1-2 days, during which clear, tense blisters develop rapidly and contain peak concentrations of infectious viral particles. This phase represents the period of maximum contagiousness and viral shedding.
Following vesicle rupture, the ulcerative phase begins as shallow, painful erosions replace the intact vesicles. These ulcers typically persist for 2-4 days before transitioning to the crusting phase, characterised by the formation of honey-coloured or dark brown scabs. The complete healing process usually requires 7-14 days, with the crusting phase gradually resolving to reveal restored epithelium. Recurrent outbreaks typically follow shorter timelines than primary infections, reflecting pre-existing immune responses to the viral antigens.
Acne vulgaris mechanics and comedonal development on lip margins
Acne lesions affecting the perioral region represent localised inflammatory responses within pilosebaceous units, involving complex interactions between sebaceous gland hyperactivity, follicular keratinisation abnormalities, and bacterial colonisation. Unlike viral infections, acne pathogenesis centres around mechanical obstruction of follicular openings and subsequent inflammatory cascades triggered by bacterial proliferation and sebum accumulation.
Sebaceous gland hyperactivity and propionibacterium acnes colonisation
The development of lip-adjacent acne lesions involves increased sebaceous gland activity, particularly in areas where pilosebaceous units exist near the vermilion border. Propionibacterium acnes , an anaerobic bacterium naturally present in follicular environments, proliferates rapidly when sebum production exceeds the follicle’s capacity for natural drainage. This bacterial overgrowth triggers inflammatory responses that manifest as the characteristic red, swollen lesions associated with acne vulgaris.
The bacterial colonisation process differs markedly from viral infections, as P. acnes represents opportunistic proliferation of commensal organisms rather than primary pathogenic invasion. This distinction explains why acne lesions lack the systematic spread patterns characteristic of viral infections and instead appear as isolated inflammatory foci within individual follicular units.
Follicular keratinisation and comedone formation mechanisms
Abnormal keratinisation within follicular channels creates the foundation for comedonal acne development through impaired sebum drainage and cellular debris accumulation. The process begins with hyperkeratinisation of the follicular epithelium, leading to the formation of keratin plugs that obstruct normal sebaceous flow. These plugs, combined with accumulated sebum and cellular debris, create the characteristic comedonal lesions that may appear as either open (blackheads) or closed (whiteheads) formations.
The mechanical nature of comedone formation contrasts with the cytolytic processes underlying herpes vesicle development. Whilst viral infections cause direct cellular destruction through replication cycles, comedonal lesions result from physical obstruction and subsequent inflammatory responses to bacterial proliferation. This fundamental difference in pathogenesis explains the distinct morphological characteristics observed in each condition.
Inflammatory response patterns in perioral acne lesions
The inflammatory cascade associated with perioral acne involves recruitment of immune cells to sites of bacterial proliferation, creating the characteristic erythema, swelling, and eventual purulent discharge observed in inflamed comedones. Neutrophil infiltration dominates the acute inflammatory response, leading to the formation of microabscesses within affected follicles. The resulting inflammatory exudate contains bacterial organisms, inflammatory cells, and cellular debris, creating the distinctive purulent content of acne lesions.
The inflammatory patterns in acne lesions reflect immune responses to bacterial proliferation rather than viral cytopathic effects, resulting in purulent rather than clear fluid accumulation within affected follicles.
This inflammatory profile differs significantly from the viral-induced tissue damage seen in herpes infections. Acne inflammation represents host defence mechanisms against bacterial overgrowth, whilst herpes inflammation results from direct viral cytotoxicity and immune recognition of infected cells. Understanding these mechanistic differences proves crucial for selecting appropriate therapeutic interventions.
Hormonal influences on lip line breakout occurrence
Hormonal fluctuations significantly impact sebaceous gland activity and can trigger acne outbreaks in the perioral region, particularly along the jawline and lower facial areas. Androgenic hormones, including testosterone and its metabolites, stimulate sebaceous gland proliferation and increase sebum production, creating favourable conditions for P. acnes colonisation. Women often experience cyclical acne flares corresponding to menstrual cycle phases, with breakouts typically occurring during luteal phase hormonal shifts.
The hormonal component of acne development provides another distinguishing feature from herpes infections, which show no correlation with endocrine fluctuations. Whilst herpes reactivation may correlate with stress-induced immunosuppression, the underlying viral pathogenesis remains independent of hormonal influences. This difference can aid in diagnostic differentiation, particularly when lesions appear in temporal patterns suggesting hormonal triggers.
Differential diagnostic criteria between viral and bacterial lesions
Establishing definitive diagnostic criteria requires systematic evaluation of multiple clinical parameters, including lesion morphology, distribution patterns, associated symptoms, and temporal characteristics. The distinction between viral and bacterial aetiologies becomes apparent through careful assessment of these diagnostic markers, each reflecting the underlying pathophysiological processes driving lesion development.
The morphological characteristics of herpes lesions evolve through predictable phases, beginning with erythematous macules that rapidly progress to vesicular eruptions. These vesicles typically measure 2-4 millimetres in diameter and contain clear, infectious fluid under considerable pressure. Upon rupture, the vesicles transform into shallow ulcers with irregular borders and erythematous halos. In contrast, acne lesions present as firm, inflammatory papules with central comedonal plugs or purulent contents. The presence of vesicular formations strongly suggests viral aetiology , as bacterial acne rarely produces true vesicles during its developmental progression.
Temporal patterns provide additional diagnostic insight, with herpes outbreaks following characteristic timelines from prodromal symptoms through complete resolution. The rapid onset of herpes lesions, typically developing within 24-48 hours of initial symptoms, contrasts with the gradual emergence of acne lesions over several days to weeks. Furthermore, herpes recurrences tend to occur in identical anatomical locations, reflecting the neurotropic nature of viral reactivation, whilst acne lesions appear randomly throughout areas containing pilosebaceous units.
| Diagnostic Feature | Herpes Simplex | Acne Vulgaris |
|---|---|---|
| Prodromal Symptoms | Tingling, burning sensation | None or mild tenderness |
| Lesion Morphology | Clear vesicles progressing to ulcers | Inflammatory papules with purulent centres |
| Fluid Content | Clear, protein-rich viral fluid | Purulent material with bacteria |
| Distribution Pattern | Consistent anatomical locations | Random follicular distribution |
| Healing Timeline | 7-14 days with crusting phase | Variable, often prolonged |
The pain characteristics associated with each condition offer additional diagnostic clues. Herpes lesions typically produce sharp, neuralgic pain that may precede visible lesion formation and intensify during the ulcerative phase. This neurological component reflects the viral infection’s impact on sensory nerve pathways. Conversely, acne lesions generate localised inflammatory pain that corresponds directly to the degree of follicular inflammation and typically lacks the neuralgic quality characteristic of viral infections.
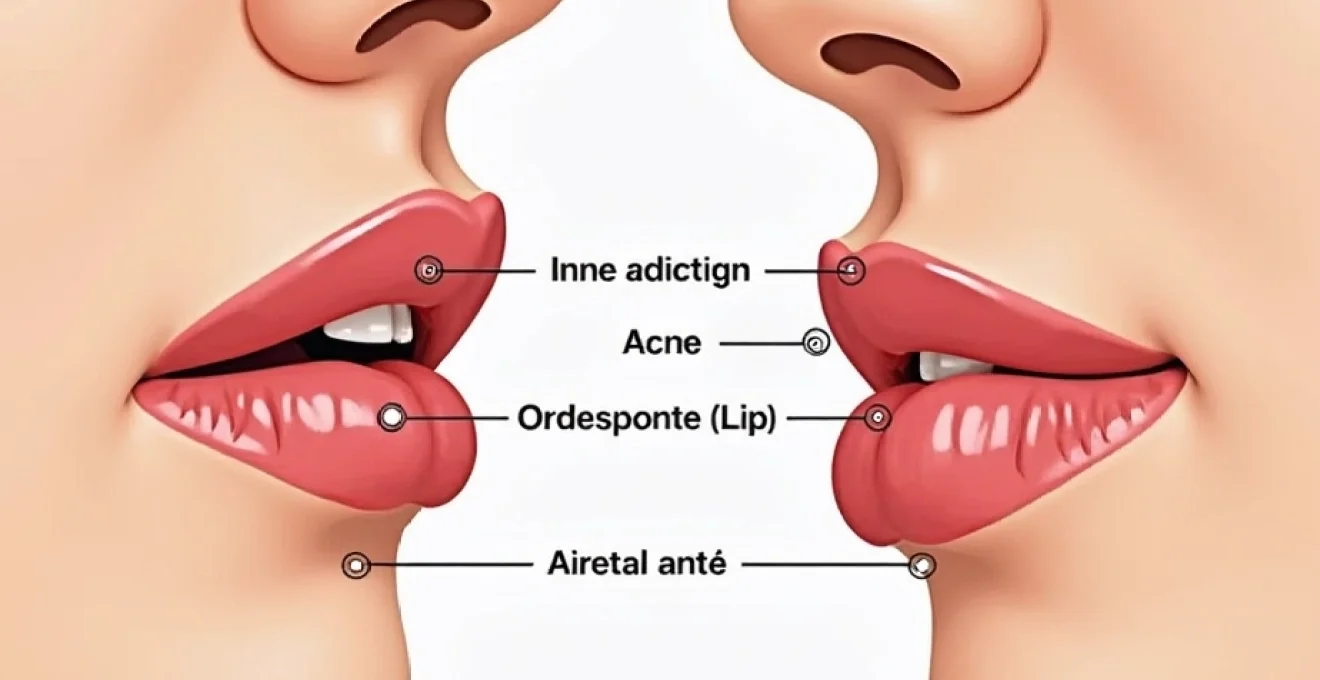
Anatomical location analysis and lesion distribution patterns
The anatomical distribution of lesions provides crucial diagnostic information, as herpes simplex virus infections and acne vulgaris demonstrate distinct predilections for specific perioral regions. Understanding these distribution patterns enables clinicians to distinguish between viral and bacterial aetiologies based on lesion location and clustering characteristics, particularly when morphological features appear ambiguous during early developmental stages.
Herpes labialis demonstrates a strong predilection for the vermilion border and adjacent skin areas innervated by the trigeminal nerve. The characteristic clustering of vesicles along specific dermatomes reflects the neurotropic nature of viral reactivation, with lesions appearing in linear or grouped arrangements following nerve pathway distributions. The consistent anatomical recurrence pattern in individual patients provides pathognomonic evidence of viral aetiology, as bacterial infections lack this neuroanatomical specificity.
Perioral acne lesions follow different distribution patterns, appearing wherever pilosebaceous units exist within the facial region. The lip margin itself contains no sebaceous glands, making true lip acne impossible; however, lesions frequently develop along the vermilion border where follicular units transition from cutaneous to mucosal tissue. These acne lesions appear as randomly distributed inflammatory papules without the clustering characteristics typical of viral infections, reflecting their origin from individual follicular units rather than viral spread along nerve pathways.
The neuroanatomical specificity of herpes lesion distribution, with consistent recurrence in identical locations, provides pathognomonic evidence distinguishing viral infections from randomly distributed bacterial acne lesions.
Secondary bacterial infections can complicate herpes lesions, particularly during the ulcerative phase when disrupted epithelium provides bacterial entry points. However, the underlying distribution pattern remains consistent with viral pathogenesis, as the initial lesion formation follows neurological rather than follicular pathways. Recognition of these anatomical principles enables accurate diagnosis even when secondary complications obscure primary morphological characteristics.
Professional medical assessment and laboratory confirmation methods
Clinical diagnosis of perioral lesions requires systematic evaluation combining visual inspection, patient history assessment, and when necessary, laboratory confirmation techniques. The diagnostic process should encompass evaluation of prodromal symptoms, lesion morphology, distribution patterns, and temporal characteristics, with laboratory testing reserved for cases presenting diagnostic uncertainty or requiring definitive viral confirmation for treatment planning purposes.
Visual inspection focuses on lesion morphology, particularly the presence or absence of vesicular formations, fluid characteristics, and clustering patterns. Healthcare providers should assess lesion borders , evaluating the scalloped edges characteristic of merged herpes vesicles versus the discrete borders typical of individual acne lesions. The fluid content examination, when safely accessible, provides additional diagnostic information, with clear, proteinaceous fluid suggesting viral aetiology and purulent material indicating bacterial involvement.
Patient history gathering should explore potential viral exposure, previous outbreak patterns, and prodromal symptom recognition. Individuals with recurrent herpes often develop familiarity with their personal outbreak characteristics, including specific prodromal sensations, typical lesion locations, and healing timelines. This historical information proves invaluable for diagnostic confirmation, particularly when combined with physical examination findings consistent with viral pathogenesis.
Laboratory confirmation methods include polymerase chain reaction (PCR) testing, viral culture, and direct fluorescent antibody staining of lesional material. PCR testing provides the highest sensitivity and specificity for herpes simplex virus detection, capable of identifying viral DNA even during later outbreak phases when viral shedding diminishes. Viral culture requires viable organisms and shows reduced sensitivity compared to molecular methods, though it enables antiviral susceptibility testing when resistance concerns exist. Direct fluorescent antibody testing offers rapid results but demonstrates lower sensitivity than molecular techniques, particularly for recurrent outbreaks with reduced viral loads.
Treatment protocol variations and antiviral versus antimicrobial approaches
The therapeutic management of perioral lesions requires distinct approaches depending on viral or bacterial aetiology, with treatment protocols differing substantially in their mechanisms of action, dosing regimens, and expected clinical outcomes. Understanding these therapeutic distinctions proves essential for optimal patient care and prevention of treatment failures resulting from inappropriate medication selection or dosing protocols.
Antiviral therapy for herpes simplex infections targets viral DNA polymerase enzymes essential for viral replication cycles. The nucleoside analogues acyclovir, valacyclovir, and famciclov
ir demonstrate superior bioavailability and dosing convenience compared to acyclovir, enabling less frequent administration while maintaining therapeutic efficacy. Topical formulations containing these antiviral agents provide localised therapy with minimal systemic exposure, though oral preparations typically demonstrate superior clinical outcomes for moderate to severe outbreaks.
The optimal timing of antiviral intervention significantly impacts treatment effectiveness, with greatest benefits achieved when therapy commences during the prodromal phase or within 24 hours of lesion appearance. Early antiviral treatment can reduce outbreak duration by 1-2 days and diminish symptom severity, though intervention beyond 48 hours of lesion onset shows limited clinical benefit. Suppressive antiviral therapy may be warranted for individuals experiencing frequent recurrent outbreaks, typically defined as six or more episodes annually.
Antimicrobial approaches for acne lesions target Propionibacterium acnes proliferation through topical antibiotics, systemic antibiotics, or combination therapy protocols. Topical preparations containing benzoyl peroxide demonstrate dual antimicrobial and comedolytic activity, making them first-line treatments for mild to moderate perioral acne. The oxidising properties of benzoyl peroxide create an unfavourable environment for anaerobic bacterial growth whilst simultaneously promoting comedonal drainage through keratolytic effects.
The fundamental difference between antiviral and antimicrobial therapies reflects the distinct pathophysiological mechanisms underlying viral replication versus bacterial proliferation in perioral lesions.
Topical retinoids represent another cornerstone of acne therapy, addressing the follicular keratinisation abnormalities that predispose to comedone formation. These vitamin A derivatives normalise follicular epithelial turnover, preventing the formation of keratin plugs that obstruct sebaceous drainage. The anti-inflammatory properties of retinoids provide additional therapeutic benefits, reducing the inflammatory cascade associated with bacterial colonisation. However, the irritant potential of retinoids requires careful patient counselling regarding proper application techniques and expected adaptation periods.
Systemic antibiotic therapy becomes necessary for inflammatory acne lesions that prove refractory to topical treatments or when lesions are too numerous for effective topical application. Tetracycline-class antibiotics demonstrate particular efficacy against P. acnes whilst providing anti-inflammatory effects independent of their antimicrobial activity. Combination therapy protocols combining topical and systemic approaches often yield superior outcomes compared to monotherapy regimens, particularly for moderate to severe inflammatory acne.
The distinction between viral and bacterial pathogenesis becomes crucial when selecting appropriate therapeutic interventions. Antiviral medications demonstrate no efficacy against bacterial acne lesions, whilst antimicrobial treatments provide no benefit for viral replication cycles. This fundamental principle underscores the importance of accurate diagnostic differentiation, as inappropriate treatment selection can lead to therapeutic failures and prolonged patient discomfort. Moreover, the contagious nature of herpes infections requires additional patient counselling regarding transmission prevention measures, a consideration unnecessary for non-infectious acne lesions.
Supportive care measures complement specific antiviral or antimicrobial therapies and can enhance patient comfort during the healing process. For herpes lesions, gentle cleansing with saline solutions and application of protective barriers such as petroleum jelly can prevent secondary bacterial infections and promote epithelial healing. Pain management through topical anaesthetics or oral analgesics may be necessary during the acute ulcerative phase, particularly for primary infections associated with more severe symptomatology.
Patient education regarding treatment expectations and potential complications forms an integral component of therapeutic management. Individuals with herpes infections require counselling about viral transmission risks, particularly during active outbreaks when viral shedding reaches peak levels. The chronic nature of herpes simplex virus infections necessitates discussion of recurrence patterns and potential trigger factors that may precipitate future outbreaks. Conversely, acne patients benefit from education about the multifactorial nature of their condition and the importance of consistent treatment adherence for optimal clinical outcomes.
The psychological impact of perioral lesions, regardless of aetiology, deserves consideration in treatment planning protocols. Both herpes infections and acne lesions can significantly affect patient self-esteem and social interactions, particularly when lesions occur in highly visible facial locations. Healthcare providers should acknowledge these psychosocial concerns and consider the cosmetic implications of various treatment options when developing individualised therapeutic regimens. The temporary nature of most perioral lesions provides reassurance to patients, though the potential for recurrence in both conditions requires ongoing management strategies.
Monitoring treatment response enables adjustment of therapeutic protocols and identification of complications requiring additional intervention. Herpes lesions should demonstrate progressive healing within 7-10 days of antiviral initiation, with failure to improve suggesting potential antiviral resistance or secondary bacterial infection. Acne lesions typically require 4-6 weeks of consistent therapy before significant improvement becomes apparent, reflecting the time required for follicular turnover and bacterial suppression. Patient follow-up appointments should assess treatment tolerance and provide opportunities for regimen modification based on clinical response patterns.