Cervical spine degeneration affecting the C5-6 and C6-7 levels represents one of the most common manifestations of age-related spinal pathology, with disc osteophyte complexes emerging as a significant clinical concern. These degenerative changes involve the formation of bony outgrowths (osteophytes) combined with intervertebral disc deterioration, creating a complex pathophysiological process that can profoundly impact neural structures and patient function. The cervical region, particularly at these transitional levels, bears considerable mechanical stress throughout daily activities, making it particularly susceptible to degenerative changes that can compromise both nerve roots and the spinal cord itself.
The development of disc osteophyte complexes at C5-6 and C6-7 typically results from a cascade of degenerative processes that begin with disc dehydration and progress to involve multiple anatomical structures. Understanding these mechanisms becomes crucial for clinicians managing patients with cervical spondylosis, as early recognition and appropriate intervention can significantly influence long-term outcomes and prevent progression to more severe neurological compromise.
Anatomical structure and pathophysiology of cervical disc osteophyte complexes
The cervical spine’s unique anatomical configuration makes the C5-6 and C6-7 levels particularly vulnerable to degenerative changes. These segments experience the greatest range of motion in the lower cervical spine, subjecting the intervertebral discs to repetitive stress cycles that gradually compromise their structural integrity. The pathophysiological process begins at the cellular level, where chronic mechanical loading leads to alterations in disc metabolism and gradual breakdown of the extracellular matrix.
Vertebral body endplate degeneration at C5-6 and C6-7 levels
Vertebral endplate degeneration serves as the initial trigger for disc osteophyte complex formation, with the cartilaginous endplates acting as the primary interface between the vertebral bodies and intervertebral discs. At the C5-6 and C6-7 levels, these endplates undergo progressive calcification and sclerosis, disrupting the normal nutrient exchange pathways that maintain disc health. This process typically begins in the third decade of life but accelerates significantly after age 50, with endplate changes visible on imaging studies preceding clinically apparent disc degeneration by several years.
The degenerative cascade involves the formation of Schmorl’s nodes, where nucleus pulposus material herniates through weakened endplates into the vertebral body. These changes create focal areas of increased mechanical stress, promoting the development of marginal osteophytes along the vertebral rim. Research indicates that endplate degeneration at C5-6 occurs approximately 15% more frequently than at other cervical levels, likely due to the biomechanical demands placed on this transitional segment.
Uncovertebral joint hypertrophy and osteophyte formation mechanisms
The uncovertebral joints, unique anatomical structures found only in the cervical spine from C3 to C7, play a crucial role in disc osteophyte complex development. These joints, also known as Luschka joints, develop during adolescence and serve to guide cervical motion while providing lateral stability. At the C5-6 and C6-7 levels, uncovertebral joint hypertrophy represents a compensatory mechanism for disc space narrowing and segmental instability.
The formation of uncovertebral osteophytes follows a predictable pattern, beginning with synovial proliferation and progressing to cartilage destruction and eventual ossification. These bony outgrowths can extend both medially and laterally, with medial extension potentially compromising the neural foramina and contributing to radicular symptoms. Studies demonstrate that uncovertebral osteophytes measuring greater than 3mm in height significantly increase the risk of nerve root compression at these levels.
Intervertebral disc space narrowing and nucleus pulposus dehydration
Progressive disc dehydration represents the hallmark of degenerative disc disease at C5-6 and C6-7, with the nucleus pulposus losing its characteristic gelatinous consistency and water content. This process, driven by decreased proteoglycan synthesis and increased collagen cross-linking, results in reduced disc height and altered load distribution across the motion segment. The normal disc height at these levels measures approximately 5-6mm, with reductions exceeding 25% considered pathologically significant.
As the nucleus pulposus dehydrates and fragments, the annulus fibrosus experiences increased mechanical stress, leading to the development of annular tears and eventual disc bulging or herniation. The combination of disc space narrowing and osteophyte formation creates what clinicians term a “disc osteophyte complex,” where it becomes difficult to distinguish between discogenic and osteophytic contributions to neural compression. Advanced imaging techniques can help differentiate these components, though treatment approaches often address both simultaneously.
Ligamentum flavum thickening and posterior longitudinal ligament ossification
Ligamentous changes accompany disc osteophyte complex formation, with the ligamentum flavum demonstrating progressive thickening and loss of elasticity. Normal ligamentum flavum thickness measures 2-3mm, but degenerative changes can result in measurements exceeding 5mm, contributing to central canal stenosis. This thickening occurs through a combination of fibrotic changes, calcification, and hypertrophic responses to chronic mechanical stress.
Posterior longitudinal ligament ossification (OPLL) represents a more severe manifestation of ligamentous degeneration, occurring in approximately 2-3% of the general population but showing higher prevalence in certain ethnic groups. When OPLL develops at C5-6 or C6-7, it can create significant spinal cord compression, particularly when combined with anterior osteophytic encroachment. The resulting “pincer” effect between anterior and posterior compressive elements can lead to severe myelopathic symptoms even with relatively modest individual contributions from each component.
Clinical manifestations and neurological compression patterns
The clinical presentation of disc osteophyte complexes at C5-6 and C6-7 varies considerably depending on the specific neural structures affected and the degree of compression present. Patients may present with isolated radicular symptoms, myelopathic signs, or a combination of both, reflecting the complex interplay between nerve root and spinal cord compression. The gradual onset typical of degenerative changes often results in symptom accommodation, with patients adapting to progressive functional limitations until reaching a critical threshold where neurological compromise becomes apparent.
C6 nerve root radiculopathy symptoms and dermatomal distribution
C6 radiculopathy, commonly resulting from disc osteophyte complexes at the C5-6 level, produces a characteristic pattern of sensory and motor symptoms that follow the C6 dermatome and myotome distribution. Patients typically experience pain radiating from the neck into the lateral arm, forearm, and thumb side of the hand, often described as burning, electric, or aching in quality. The pain frequently worsens with neck extension and lateral bending toward the affected side, as these movements further narrow the neural foramen.
Motor symptoms include weakness in biceps function, wrist extension, and thumb extension, reflecting the C6 myotome distribution. The biceps reflex may be diminished or absent, providing an important clinical sign for localising the level of pathology. Sensory changes typically affect the lateral forearm and thumb, though the exact distribution can vary among individuals. Provocative testing such as Spurling’s manoeuvre often reproduces radicular symptoms, helping to confirm the diagnosis and differentiate nerve root compression from other causes of arm pain.
C7 nerve root compression effects on triceps and finger extensors
C7 radiculopathy, most commonly associated with C6-7 disc osteophyte complexes, presents with distinct clinical features that differ from C6 involvement. The pain pattern typically follows the posterior arm and forearm, extending into the middle finger region. Patients often report difficulty with pushing motions and overhead activities, reflecting weakness in the triceps and finger extensors that characterise C7 myotome dysfunction.
The triceps reflex serves as a key diagnostic indicator, often showing diminution or absence in cases of significant C7 nerve root compression. Motor testing reveals weakness in elbow extension, wrist flexion, and finger extension, with the middle finger extension being particularly affected. Sensory changes typically involve the middle finger and surrounding areas, though overlap with adjacent dermatomes can complicate clinical assessment. Functional limitations often include difficulty with typing, writing, and fine motor tasks that require coordinated finger extension.
Cervical myelopathy development through central canal stenosis
When disc osteophyte complexes at C5-6 and C6-7 result in significant central canal narrowing, cervical myelopathy can develop, representing a more serious neurological condition than isolated radiculopathy. The normal cervical spinal canal measures 17-18mm in the sagittal diameter, with stenosis considered significant when measurements fall below 13mm. The combination of anterior osteophytic encroachment and posterior ligamentous hypertrophy can create a “pincer” effect that progressively compresses the spinal cord.
Early myelopathic symptoms include hand clumsiness, difficulty with fine motor tasks, and gait instability. Patients may notice problems with buttoning clothes, writing, or using utensils, reflecting upper motor neuron dysfunction. As the condition progresses, lower extremity symptoms develop, including leg weakness, balance problems, and potential bowel or bladder dysfunction in severe cases. Hoffmann’s sign and hyperreflexia in the lower extremities provide important clinical indicators of myelopathic involvement and help distinguish this condition from isolated radiculopathy.
Vertebrobasilar insufficiency secondary to foraminal narrowing
Although less common, severe foraminal narrowing from disc osteophyte complexes can occasionally compromise the vertebral arteries as they course through the transverse foramina. This anatomical relationship becomes clinically relevant when osteophytic growth extends laterally enough to impinge upon these vessels, potentially contributing to vertebrobasilar insufficiency symptoms. Patients may experience dizziness, vertigo, or visual disturbances, particularly with certain neck movements that further compromise vascular flow.
The clinical diagnosis of vertebrobasilar insufficiency secondary to cervical pathology requires careful correlation between symptoms and imaging findings, as multiple factors can contribute to these complaints. Dynamic studies, including CT angiography with neck positioning, may help identify cases where osteophytic compression significantly affects vertebral artery flow. However, surgical intervention for vascular compression remains controversial and is typically reserved for cases with clear imaging evidence and refractory symptoms.
Advanced diagnostic imaging techniques for cervical osteophyte assessment
Accurate assessment of disc osteophyte complexes at C5-6 and C6-7 requires sophisticated imaging approaches that can differentiate between various pathological components and guide appropriate treatment decisions. Modern imaging protocols have evolved significantly, incorporating advanced MRI sequences, specialised CT techniques, and dynamic studies that provide comprehensive evaluation of both static and functional aspects of cervical spine pathology. The integration of multiple imaging modalities allows clinicians to develop detailed understanding of the pathoanatomical changes and their relationship to clinical symptoms.
MRI T2-Weighted sagittal sequences for disc signal changes
T2-weighted sagittal MRI sequences serve as the gold standard for evaluating disc degeneration and associated signal changes in cervical disc osteophyte complexes. Normal intervertebral discs demonstrate high signal intensity on T2-weighted images due to their high water content, while degenerative changes result in progressive signal loss that correlates with the severity of pathological changes. The Pfirrmann grading system, widely used for lumbar discs, has been adapted for cervical spine assessment, providing standardised criteria for quantifying degenerative changes.
At the C5-6 and C6-7 levels, T2-weighted imaging can identify disc dehydration, annular tears, and the relationship between disc material and surrounding neural structures. High-intensity zones within the posterior annulus may indicate annular tears that could be sources of neck pain, while disc protrusions or extrusions can be clearly delineated from surrounding osteophytic changes. Multiplanar imaging reconstruction allows for precise measurement of canal dimensions and assessment of neural foraminal compromise, providing crucial information for surgical planning when conservative treatment fails.
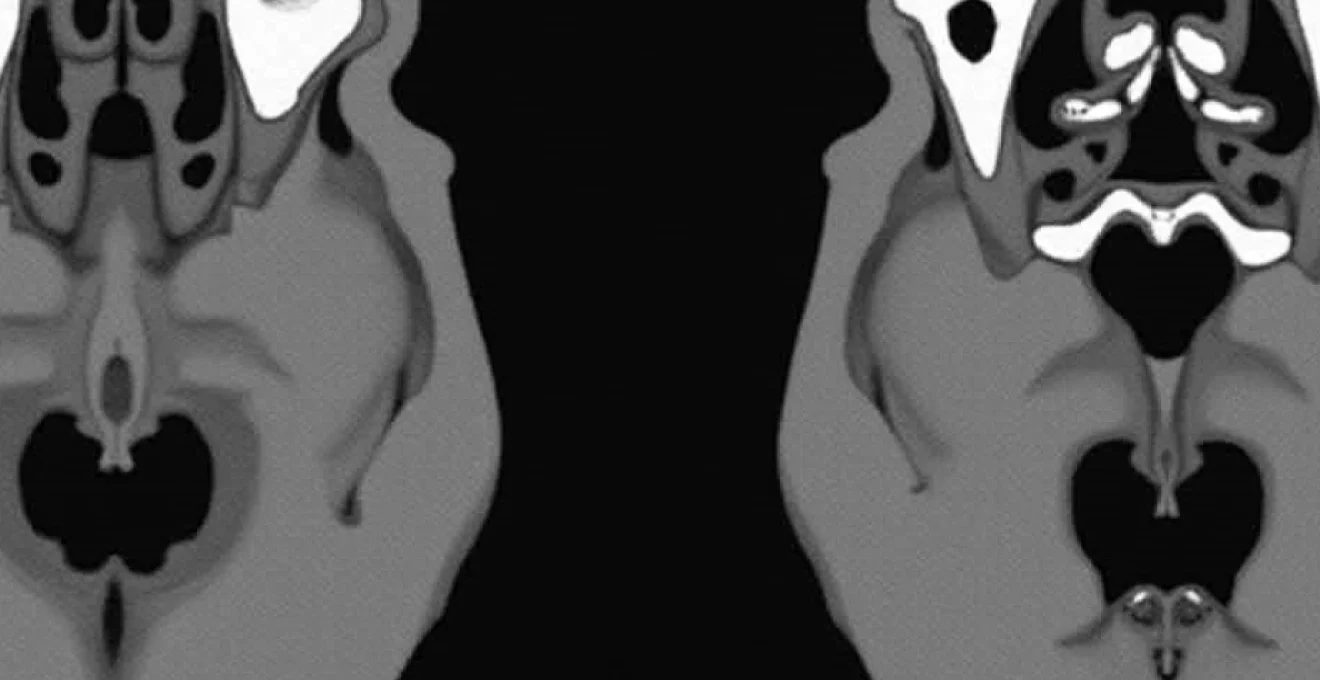
CT myelography protocol for neural foraminal stenosis evaluation
CT myelography remains an invaluable tool for assessing neural foraminal stenosis in cases where MRI findings are equivocal or when precise bony detail is required for surgical planning. This technique combines the excellent bony resolution of CT with contrast enhancement of neural structures, allowing for detailed assessment of both soft tissue and osseous contributions to neural compression. The procedure involves intrathecal contrast injection followed by CT imaging in multiple positions, providing dynamic information about neural compression patterns.
For C5-6 and C6-7 disc osteophyte complexes, CT myelography can precisely delineate the degree of foraminal narrowing and identify the specific anatomical structures responsible for nerve root compression. The technique is particularly valuable in distinguishing between anterior osteophytic compression and lateral disc herniation, information that directly impacts surgical approach selection. Three-dimensional reconstructions from CT myelography data can provide surgeons with detailed anatomical roadmaps, particularly useful in complex cases involving multilevel pathology or previous surgical intervention.
STIR sequences for bone marrow oedema detection
Short-tau inversion recovery (STIR) sequences offer superior sensitivity for detecting bone marrow oedema and inflammatory changes associated with disc osteophyte complexes. These sequences suppress fat signal while enhancing fluid signal, making them particularly useful for identifying active inflammatory processes within vertebral bodies and endplates. STIR imaging can reveal Modic changes, which represent different stages of endplate and marrow pathology associated with disc degeneration.
Type I Modic changes, characterised by bone marrow oedema and inflammatory infiltration, appear as decreased signal on T1-weighted images and increased signal on STIR sequences. These changes often correlate with clinical symptoms and may indicate active degenerative processes that could respond to anti-inflammatory treatments. At C5-6 and C6-7 levels, STIR signal changes can help identify patients who might benefit from targeted interventions such as epidural steroid injections or specific pharmaceutical approaches aimed at reducing inflammatory activity.
Dynamic Flexion-Extension radiographs for instability assessment
Dynamic flexion-extension radiographs provide crucial information about segmental stability at levels affected by disc osteophyte complexes. While degenerative changes typically result in decreased motion, some patients may develop segmental instability, particularly in the early stages of disc degeneration before significant osteophytic bridging occurs. These studies involve obtaining lateral cervical spine radiographs in maximum flexion and extension positions, allowing measurement of segmental motion and identification of abnormal translation or angulation.
Normal cervical spine flexion-extension demonstrates approximately 15-20 degrees of motion at each level, with translation limited to 2mm or less. At C5-6 and C6-7 levels, excessive motion may indicate ligamentous laxity or disc disruption that could contribute to symptom generation and influence treatment recommendations. Conversely, significantly reduced motion may suggest advanced degenerative changes with functional ankylosis. Digital motion radiography represents an advanced technique that can provide real-time assessment of segmental motion patterns, offering insights into functional pathology that static imaging cannot reveal.
Conservative treatment protocols and interventional pain management
Conservative management represents the first-line approach for most patients with disc osteophyte complexes at C5-6 and C6-7, with evidence supporting non-operative treatment for the majority of cases. Comprehensive conservative protocols integrate multiple therapeutic modalities, including physical therapy, pharmacological interventions, lifestyle modifications, and targeted injection procedures. The success of conservative treatment depends largely on early intervention, patient compliance, and appropriate selection of treatment components based on the specific pathophysiological processes involved.
Physical therapy forms the cornerstone of conservative management, focusing on cervical stabilisation exercises, postural correction, and mobility enhancement. Therapeutic protocols typically begin with pain and inflammation control, progressing through range-of-motion restoration and finally advancing to strengthening and functional rehabilitation. Manual therapy techniques , including mobilisation and manipulation, can provide symptomatic relief while
improving muscle flexibility and reducing mechanical stress on affected segments. Cervical traction, both manual and mechanical, can provide temporary decompression of neural structures while promoting healing of inflamed tissues.
Pharmacological interventions target both pain control and inflammatory reduction, with NSAIDs serving as first-line medications for most patients. Muscle relaxants may provide additional benefit during acute exacerbations, while neuropathic pain medications such as gabapentin or pregabalin can address radicular symptoms more effectively than traditional analgesics. Corticosteroid medications may be considered for short-term use during severe inflammatory episodes, though long-term use should be avoided due to potential adverse effects on bone health and healing processes.
Interventional pain management procedures offer targeted relief for patients who fail to respond adequately to conservative measures. Cervical epidural steroid injections represent the most commonly employed interventional technique, with success rates ranging from 60-80% for radicular symptoms. These procedures involve precise needle placement under fluoroscopic guidance, allowing delivery of anti-inflammatory medications directly to the affected neural structures. The timing of injection therapy is crucial, with optimal results achieved when performed during active inflammatory phases rather than in cases of pure mechanical compression.
Cervical facet joint injections and medial branch blocks may provide additional therapeutic options for patients with predominant axial neck pain related to facet joint arthropathy. Radiofrequency ablation of medial branches can offer longer-lasting relief for carefully selected patients, though the proximity of neural structures in the cervical spine requires exceptional technical precision. Selective nerve root blocks serve both diagnostic and therapeutic purposes, helping to identify the specific nerve root responsible for symptoms while providing targeted pain relief that may facilitate participation in rehabilitation programs.
Surgical intervention strategies and fusion techniques
Surgical intervention for disc osteophyte complexes at C5-6 and C6-7 becomes necessary when conservative treatment fails to provide adequate symptom relief or when progressive neurological deterioration occurs. The decision for surgical intervention requires careful consideration of multiple factors, including symptom severity, neurological signs, imaging findings, and patient expectations. Modern surgical techniques offer various approaches, each with specific advantages and limitations that must be weighed against individual patient characteristics and pathoanatomical findings.
Anterior cervical discectomy and fusion (ACDF) remains the gold standard surgical procedure for addressing disc osteophyte complexes with significant anterior neural compression. This approach allows direct visualization and removal of both disc material and osteophytic growths that contribute to neural compression. The procedure involves complete discectomy, thorough decompression of neural foramina, and placement of an interbody graft or cage to maintain disc height and restore normal alignment. Titanium plates and screws provide additional stability and promote fusion, though some surgeons prefer standalone cages in select cases to minimize implant-related complications.
The success of ACDF procedures depends heavily on proper patient selection and meticulous surgical technique. Fusion rates exceed 95% for single-level procedures, though two-level fusions may have slightly lower success rates. Clinical outcomes demonstrate excellent pain relief in 80-90% of patients, with neurological improvement occurring in the majority of cases when surgery is performed before irreversible nerve damage develops. However, adjacent segment disease remains a concern, with studies showing 15-20% of patients developing symptomatic degeneration at levels adjacent to the fusion within 10 years.
Cervical disc replacement (arthroplasty) has emerged as an alternative to fusion for carefully selected patients with disc osteophyte complexes. This motion-preserving technique aims to maintain segmental mobility while addressing neural compression, potentially reducing the risk of adjacent segment degeneration. Current artificial disc designs demonstrate good short-term outcomes, though long-term data remains limited. Patient selection criteria are more restrictive than for ACDF, requiring preserved facet joints, adequate bone quality, and absence of significant instability or deformity.
Posterior surgical approaches, including laminoplasty and laminectomy with fusion, may be considered for patients with predominant central canal stenosis or when multiple levels require decompression. Laminoplasty preserves the posterior elements while creating additional space for the spinal cord, making it particularly suitable for patients with cervical myelopathy due to multilevel stenosis. However, posterior approaches may not adequately address anterior compression from disc osteophyte complexes, and some patients may experience post-operative axial neck pain or loss of cervical lordosis.
Minimally invasive surgical techniques continue to evolve, offering potential advantages including reduced tissue trauma, faster recovery, and improved cosmetic outcomes. These approaches require specialized instrumentation and training but may provide comparable decompression with less morbidity than traditional open procedures. Endoscopic discectomy techniques show promise for treating certain types of cervical disc pathology, though their application to complex osteophytic disease remains limited.
Long-term prognosis and adjacent segment degeneration prevention
The long-term prognosis for patients with disc osteophyte complexes at C5-6 and C6-7 varies significantly based on the severity of initial presentation, treatment approach, and individual patient factors. Natural history studies indicate that many patients experience symptom improvement over time with conservative treatment, though complete resolution is less common in cases with significant structural pathology. Understanding prognostic factors helps clinicians counsel patients appropriately and develop realistic treatment expectations that account for both potential benefits and limitations of various interventions.
Patients treated conservatively generally demonstrate good symptomatic improvement, with approximately 70-80% experiencing significant pain reduction within 6-12 months. However, radiographic progression of degenerative changes continues regardless of symptom improvement, reflecting the underlying pathophysiological processes that drive disc osteophyte complex formation. Functional outcomes tend to correlate more closely with symptom severity than with radiographic findings, emphasizing the importance of patient-reported outcome measures in assessing treatment success.
Surgical outcomes demonstrate excellent short-term results, with most patients experiencing significant improvement in radicular pain and neurological symptoms. Long-term studies reveal sustained benefit in 80-85% of patients at 5-year follow-up, though some degree of symptom recurrence is not uncommon. Factors associated with superior long-term outcomes include younger age at surgery, absence of workers’ compensation issues, non-smoking status, and single-level pathology. Patients with significant psychological comorbidities or chronic pain syndromes may experience less favorable outcomes regardless of the technical success of the procedure.
Adjacent segment degeneration represents one of the most significant long-term concerns following cervical fusion procedures. While some degree of adjacent level changes occurs naturally with aging, fusion procedures may accelerate degenerative processes at unfused levels through altered biomechanics and increased stress concentration. The incidence of symptomatic adjacent segment disease ranges from 10-25% within the first decade following surgery, with higher rates observed in patients with pre-existing degenerative changes at adjacent levels.
Prevention strategies for adjacent segment degeneration focus on maintaining normal cervical alignment, preserving as much motion as possible, and addressing modifiable risk factors. Motion-preserving surgical techniques such as disc replacement may reduce adjacent segment stress, though long-term comparative studies are still needed to confirm this theoretical advantage. Non-surgical prevention strategies include maintaining good cervical posture, regular exercise to support neck musculature, smoking cessation, and management of inflammatory conditions that may accelerate degenerative processes.
The role of genetic factors in disc degeneration continues to be elucidated, with certain genetic polymorphisms associated with accelerated degenerative changes and potentially poorer treatment outcomes. As our understanding of these factors improves, personalized treatment approaches may emerge that account for individual genetic predisposition to degenerative disease. Until such advances become clinically available, emphasis remains on optimizing modifiable risk factors and selecting appropriate treatment strategies based on current evidence and individual patient characteristics.
Patient education plays a crucial role in long-term success, regardless of treatment approach. Understanding the degenerative nature of disc osteophyte complexes helps patients maintain realistic expectations while encouraging adherence to preventive measures and rehabilitation programs. Regular follow-up care allows for early identification of symptom recurrence or progression, enabling timely intervention before significant functional decline occurs. Multidisciplinary care coordination between spine specialists, physical therapists, and primary care providers ensures comprehensive management that addresses both immediate symptoms and long-term spine health maintenance.