The prominent bony bump that develops at the base of your big toe represents one of the most common foot deformities affecting millions of people worldwide. This condition, medically known as hallux valgus, creates a distinctive angular deviation where the big toe gradually tilts towards the smaller toes whilst the first metatarsal bone shifts in the opposite direction. The resulting protrusion forms what most people recognise as a bunion, though the underlying biomechanical changes extend far beyond this visible bump.
Understanding why this bone protrusion develops requires examining the complex interplay between genetic predisposition, mechanical stress, and anatomical variations that affect foot structure. The progression from normal toe alignment to significant deformity typically occurs over years, with symptoms ranging from mild cosmetic concerns to debilitating pain that severely impacts daily activities. Modern medical approaches offer comprehensive treatment strategies, from conservative management techniques to advanced surgical interventions, each tailored to address the specific severity and characteristics of individual cases.
Hallux valgus pathophysiology and anatomical deformity mechanisms
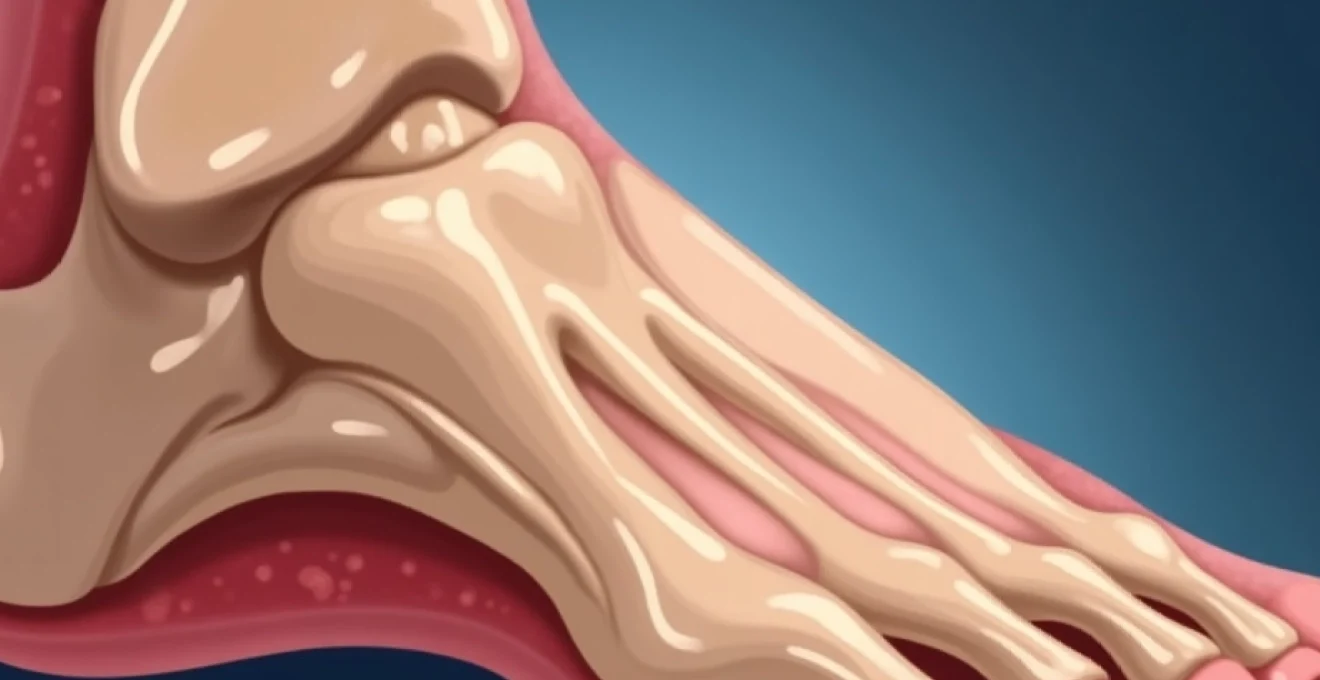
The development of a protruding big toe bone involves a complex cascade of biomechanical changes that fundamentally alter the normal architecture of the forefoot. At its core, hallux valgus represents a three-dimensional deformity affecting not only the visible angulation of the big toe but also the rotational positioning and load distribution across the entire first ray. The pathophysiology begins with subtle changes in weight-bearing patterns that gradually overwhelm the natural stabilising mechanisms of the foot.
Metatarsophalangeal joint biomechanical dysfunction in bunion formation
The metatarsophalangeal joint serves as the primary articulation point where bunion formation occurs, functioning as a complex hinge mechanism that must accommodate both sagittal plane motion during walking and transverse plane stability during weight-bearing. When this joint experiences abnormal stress patterns, the surrounding soft tissue structures begin to adapt in ways that ultimately compromise normal alignment. The joint capsule stretches on the medial side whilst contracting laterally, creating an imbalance that perpetuates the deformity progression.
Progressive changes in the joint’s articular surfaces contribute significantly to the clinical presentation of bunion deformity. The metatarsal head undergoes adaptive remodelling, developing enlarged areas of bone formation that create the characteristic bump appearance. Simultaneously, the proximal phalanx experiences altered contact patterns that can lead to degenerative changes resembling osteoarthritis, particularly in advanced cases where conservative management has been unsuccessful.
First ray hypermobility and medial cuneiform instability patterns
Excessive mobility within the first ray complex represents a fundamental predisposing factor for bunion development, as increased motion allows abnormal forces to act upon the metatarsophalangeal joint during weight-bearing activities. This hypermobility often stems from congenital variations in ligament laxity or acquired weakness in the supporting structures that normally maintain proper alignment. The medial cuneiform bone plays a crucial role in this process, as its stability directly influences the positioning of the first metatarsal bone.
When medial cuneiform instability occurs, the first metatarsal tends to drift into an abnormal position characterised by elevation and medial angulation. This malpositioning creates a mechanical disadvantage that places excessive stress on the metatarsophalangeal joint, initiating the progressive changes that eventually manifest as a visible bunion deformity. Understanding these underlying instability patterns proves essential for selecting appropriate treatment strategies that address root causes rather than merely treating symptoms.
Progressive lateral deviation of the hallux and valgus angulation measurement
The hallux valgus angle represents the most clinically significant measurement for assessing bunion severity, typically measured as the angle between the longitudinal axes of the first metatarsal and proximal phalanx on weight-bearing radiographs. Normal alignment maintains this angle below 15 degrees, whilst mild deformities present angles between 15-30 degrees, moderate cases range from 30-40 degrees, and severe deformities exceed 40 degrees. These measurements directly correlate with symptom severity and treatment complexity.
As lateral deviation progresses, secondary deformities frequently develop in adjacent toes, particularly the second digit which may develop hammer toe configuration due to crowding and altered mechanics. The progression rate varies significantly between individuals, with some experiencing rapid deterioration whilst others maintain stable deformity for years. Factors influencing progression include activity level, footwear choices, body weight, and underlying connective tissue characteristics.
Sesamoid bone displacement and plantar plate insufficiency
The sesamoid bones beneath the first metatarsal head play crucial roles in normal toe function, acting as fulcrums for flexor tendon efficiency whilst providing mechanical protection for underlying structures. In bunion deformity, these small bones undergo significant positional changes, typically displacing laterally as the metatarsal head shifts medially. This displacement creates functional deficits that contribute to pain and reduced push-off strength during walking.
Plantar plate insufficiency frequently accompanies sesamoid displacement, as the fibrous structure that normally maintains proper joint relationships becomes stretched and weakened. This insufficiency manifests as increased joint mobility, reduced stability during weight-bearing, and altered pressure distribution across the forefoot. The combination of sesamoid displacement and plantar plate weakness creates a cycle of progressive instability that accelerates bunion development and complicates treatment planning.
Clinical assessment techniques for protruding big toe bone evaluation
Comprehensive evaluation of big toe bone protrusion requires systematic assessment incorporating both clinical examination techniques and advanced imaging modalities. The diagnostic process must differentiate between primary bunion deformity and secondary changes resulting from other conditions such as inflammatory arthritis or traumatic injuries. Modern assessment protocols emphasise weight-bearing evaluation to accurately capture the functional impact of the deformity on daily activities and gait patterns.
Manchester scale grading system for hallux valgus severity
The Manchester Scale provides a standardised photographic grading system that allows clinicians to assess bunion severity using visual reference images representing four distinct grades of deformity. Grade 1 indicates no deformity with normal toe alignment, Grade 2 represents mild deformity with slight angulation, Grade 3 demonstrates moderate deformity with obvious deviation, and Grade 4 shows severe deformity with significant overlap or underlap of adjacent toes. This system offers excellent inter-observer reliability whilst providing patients with clear visual understanding of their condition severity.
Clinical application of the Manchester Scale proves particularly valuable for tracking progression over time and communicating treatment recommendations to patients. The photographic standards eliminate subjective interpretation whilst providing consistent documentation methods across different healthcare providers. Research demonstrates strong correlation between Manchester Scale grades and both radiographic measurements and patient-reported outcome scores, validating its clinical utility in bunion assessment protocols.
Weight-bearing radiographic analysis using hardy and clapham method
Weight-bearing radiographs represent the gold standard for bunion assessment, as non-weight-bearing images significantly underestimate deformity severity and fail to capture the true functional impact of the condition. The Hardy and Clapham method establishes standardised measurement techniques for key angular relationships, including the hallux valgus angle, intermetatarsal angle, and distal metatarsal articular angle. These measurements guide treatment selection whilst providing objective documentation of deformity progression.
Proper radiographic technique requires specific positioning protocols to ensure measurement accuracy and reproducibility. The anteroposterior view must be obtained with the patient standing and equal weight distribution between both feet, whilst the X-ray beam remains perpendicular to the floor. Lateral views provide additional information regarding sagittal plane alignment and can reveal associated conditions such as metatarsus primus elevatus or plantar flexed first ray positioning that influence treatment planning.
Intermetatarsal angle measurement and hallux valgus angle documentation
The intermetatarsal angle between the first and second metatarsals provides crucial information regarding the underlying deformity pattern and guides surgical planning for cases requiring operative intervention. Normal intermetatarsal angles measure less than 9 degrees, whilst mild increases range from 9-13 degrees, moderate increases span 13-20 degrees, and severe deformity presents angles exceeding 20 degrees. This measurement directly influences surgical technique selection and determines whether proximal or distal corrections prove most appropriate.
Documentation accuracy requires consistent measurement techniques using standardised anatomical landmarks and measurement protocols. The intermetatarsal angle measurement utilises the longitudinal axes of the first and second metatarsal shafts, drawn through the midpoints of the bone at proximal and distal reference points. Digital measurement systems enhance accuracy whilst reducing inter-observer variation compared to traditional manual measurement methods using goniometers or protractors.
Physical examination protocols including thompson test and windlass mechanism
Comprehensive physical examination must assess both static alignment and dynamic function to fully characterise the bunion deformity and identify contributing factors. The Thompson test evaluates first ray mobility by applying dorsal and plantar directed forces whilst measuring the range of motion available at the first metatarsocuneiform joint. Excessive mobility indicates underlying instability that may require specific surgical addressing during treatment planning.
Assessment of the windlass mechanism evaluates the functional integrity of the plantar fascia and its role in maintaining foot stability during push-off activities. This test involves passive dorsiflexion of the hallux whilst observing arch height changes and assessing the patient’s ability to maintain proper foot alignment. Dysfunction in the windlass mechanism often correlates with progressive bunion development and influences the selection of appropriate treatment strategies, particularly regarding the need for arch support or orthotic intervention.
Conservative treatment modalities for big toe bone protrusion management
Non-operative management remains the first-line treatment approach for most bunion cases, particularly those with mild to moderate deformity and manageable symptoms. Conservative strategies focus on reducing pain, preventing progression, and improving functional capacity through targeted interventions that address both mechanical and inflammatory components of the condition. Success rates for conservative management vary significantly based on deformity severity, patient compliance, and individual anatomical factors, with many patients achieving substantial symptom relief without requiring surgical intervention.
The foundation of conservative treatment involves footwear modification and patient education regarding proper shoe selection criteria. Shoes with adequate toe box width, low heel heights, and appropriate arch support can dramatically reduce symptoms whilst preventing further deformity progression. Custom orthotics play crucial roles in redistributing pressure away from prominent areas whilst providing biomechanical correction for underlying foot dysfunction. These devices must be precisely fabricated based on individual foot measurements and gait analysis to achieve optimal therapeutic benefits.
Physical therapy interventions target muscle imbalances and joint mobility restrictions that contribute to bunion development and symptom persistence. Specific exercises focus on strengthening intrinsic foot muscles, improving hallux range of motion, and addressing compensatory movement patterns that develop secondary to the deformity. Manual therapy techniques including joint mobilisation and soft tissue release can provide significant pain relief whilst improving functional capacity for daily activities.
Conservative management proves most effective when implemented early in the deformity progression, before significant structural changes limit the potential for non-operative improvement.
Anti-inflammatory medications offer symptomatic relief during acute symptom flares, though long-term use requires careful monitoring for potential adverse effects. Topical preparations may provide localised benefits with reduced systemic exposure, particularly beneficial for elderly patients with multiple medical conditions. Injection therapy using corticosteroids can provide temporary relief for severe inflammatory episodes, though repeated injections carry risks of soft tissue atrophy and should be used judiciously.
Activity modification represents an essential component of conservative management, involving identification and elimination of aggravating factors whilst maintaining appropriate activity levels for overall health. Low-impact exercises such as swimming and cycling can maintain cardiovascular fitness without exacerbating bunion symptoms. Patients must understand that complete activity restriction proves counterproductive, as deconditioning leads to muscle weakness and joint stiffness that ultimately worsen functional outcomes.
Surgical intervention options for severe hallux valgus deformity
Surgical correction becomes necessary when conservative measures fail to provide adequate symptom relief or when deformity severity significantly impacts quality of life and functional capacity. Modern bunion surgery encompasses over 100 described techniques, each designed to address specific anatomical variations and deformity patterns. Selection of appropriate surgical procedures requires careful consideration of deformity severity, patient age and activity level, bone quality, and associated foot conditions that may influence outcomes.
The primary goals of bunion surgery include pain relief, deformity correction, and restoration of normal foot function whilst minimising complications and recovery time. Success rates for appropriately selected procedures exceed 90% for patient satisfaction, though specific outcomes vary based on surgical technique, surgeon experience, and patient factors. Modern techniques emphasise anatomical restoration whilst preserving joint motion and maintaining long-term stability.
Chevron osteotomy technique for mild to moderate bunion correction
The Chevron osteotomy represents one of the most commonly performed bunion correction procedures, particularly effective for mild to moderate deformities with intermetatarsal angles below 15 degrees. This technique involves creating a V-shaped cut through the metatarsal head, allowing lateral displacement of the distal fragment to reduce the prominent bump whilst correcting angular alignment. The inherent stability of the chevron configuration typically eliminates the need for internal fixation, though modern practice increasingly utilises small screws to enhance healing and allow earlier weight-bearing.
Technical execution requires precise osteotomy planning to achieve optimal correction whilst preserving adequate bone stock for healing. The angle and orientation of the osteotomy cuts directly influence the amount of correction possible, with most surgeons planning for 60-degree included angles to maximise lateral displacement potential. Soft tissue balancing accompanies the bony correction, involving medial capsule repair and lateral soft tissue release to maintain proper alignment during healing.
Scarf osteotomy procedure and Z-Shaped bone cut implementation
The Scarf osteotomy utilises a Z-shaped cut through the metatarsal shaft, providing exceptional versatility for correcting moderate to severe bunion deformities whilst maintaining excellent bone contact for reliable healing. This technique allows multi-planar correction including lateral translation, angular correction, shortening or lengthening, and rotational adjustment as needed for individual deformity patterns. The large bone contact area promotes rapid healing whilst the stable configuration allows early mobilisation and faster recovery compared to many alternative procedures.
Surgical planning for Scarf osteotomy requires detailed preoperative analysis to determine optimal correction parameters and avoid common complications such as troughing or inadvertent shortening. The procedure demands meticulous attention to soft tissue handling and bone preparation to achieve ideal fragment positioning. Modern techniques incorporate rigid internal fixation using cortical screws or plates to eliminate post-operative displacement risks and enable accelerated rehabilitation protocols.
Lapidus fusion surgery for first tarsometatarsal joint arthrodesis
The Lapidus procedure addresses bunion deformity at its origin by fusing the first tarsometatarsal joint, providing the most powerful correction available for severe deformities with significant hypermobility. This technique proves particularly valuable for cases with intermetatarsal angles exceeding 15 degrees or when recurrent deformity has occurred following previous surgery. Arthrodesis eliminates the source of instability whilst allowing substantial angular correction that exceeds the capabilities of most osteotomy procedures.
Success of Lapidus fusion depends heavily on achieving solid bone healing, typically requiring 8-12 weeks of protected weight-bearing to ensure optimal outcomes. Modern techniques utilise advanced fixation methods including compression plates and multiple screw configurations to enhance fusion rates whilst reducing healing times. Patient selection proves critical, as the procedure works best in younger, active individuals with good bone quality and realistic expectations regarding recovery timelines.
Mitchell osteotomy and lateral soft tissue release protocols
The Mitchell osteotomy provides reliable correction for moderate bunion deformities through a horizontal cut across the metatarsal neck combined with lateral displacement and angle correction. This procedure offers predictable results with relatively straightforward surgical technique, making it particularly suitable for surgeons with developing bunion surgery experience. The horizontal osteotomy orientation allows excellent control over correction parameters whilst maintaining adequate bone contact for healing.
Lateral soft tissue release accompanies most bunion correction procedures, involving division of tight structures that contribute to deformity maintenance. The release typically includes the adductor hallucis tendon, lateral joint capsule, and occasionally the lateral head of the flexor hallucis brevis muscle. Proper soft tissue balancing proves essential for maintaining correction whilst avoiding overcorrection complications such as hallux varus or cock-up deformity.
Differential diagnosis of big toe bone prominence conditions
Accurate diagnosis requires differentiation between primary hallux valgus and other conditions that may present with similar big toe prominence or pain patterns. Gouty arthritis frequently affects the first metatarsophalangeal joint
, presenting with acute onset of severe pain, redness, and swelling that may initially appear similar to bunion inflammation. However, gout typically develops rapidly over hours rather than the gradual progression characteristic of hallux valgus deformity. Laboratory testing revealing elevated uric acid levels and characteristic crystal deposits on joint aspiration helps confirm gouty arthritis diagnosis.
Sesamoid disorders represent another important differential consideration, as these small bones beneath the first metatarsal head can develop inflammatory conditions, stress fractures, or avascular necrosis that produce localised pain and swelling. Unlike bunion deformity, sesamoid pathology typically presents with plantar-based symptoms rather than medial prominence, though concurrent conditions may coexist in complex cases. Advanced imaging including MRI or bone scan may prove necessary to differentiate between these conditions.
Hallux rigidus affects the same joint as bunion deformity but presents primarily with stiffness and pain during toe dorsiflexion rather than angular deviation. This degenerative condition involves progressive loss of joint motion due to arthritis, often accompanied by dorsal bone spur formation that creates a different pattern of prominence compared to the medial bump characteristic of hallux valgus. Clinical examination reveals restricted range of motion as the primary finding rather than angular malalignment.
Inflammatory arthropathies including rheumatoid arthritis and psoriatic arthritis frequently affect the first metatarsophalangeal joint, producing swelling and deformity that may resemble bunion formation. These systemic conditions typically present with bilateral symmetrical involvement and concurrent symptoms in other joints throughout the body. Laboratory markers including rheumatoid factor and anti-CCP antibodies help establish the diagnosis, whilst the presence of morning stiffness and systemic symptoms distinguishes these conditions from isolated bunion deformity.
Stress fractures of the first metatarsal can produce localised pain and swelling that mimics bunion symptoms, particularly in athletes or individuals with sudden increases in activity levels. The absence of angular deformity and the presence of focal tenderness over the fracture site help differentiate this condition. Advanced imaging including MRI or bone scan may be required when plain radiographs appear normal despite clinical suspicion of stress fracture.
Post-treatment rehabilitation and long-term prognosis considerations
Successful rehabilitation following bunion treatment requires comprehensive planning that addresses both the immediate post-treatment period and long-term maintenance of achieved corrections. The rehabilitation approach varies significantly between conservative and surgical management, with surgical cases requiring structured protocols that protect healing tissues whilst gradually restoring normal function. Understanding the timeline and expectations for recovery helps patients maintain realistic goals whilst maximising their potential for optimal outcomes.
Conservative treatment rehabilitation focuses on activity modification, progressive exercise protocols, and ongoing monitoring for deformity progression. Patients must understand that conservative measures typically provide symptom relief rather than structural correction, making long-term compliance with recommended interventions essential for maintaining benefits. Regular follow-up assessments allow healthcare providers to adjust treatment strategies based on symptom response and functional improvements.
Post-surgical rehabilitation follows carefully structured protocols designed to protect the surgical repair whilst progressively restoring normal foot function. The initial phase typically involves 2-6 weeks of protected weight-bearing, depending on the specific procedure performed and individual healing characteristics. During this period, patients must maintain proper foot elevation, ice application, and wound care protocols to optimise healing conditions whilst preventing complications such as infection or hardware displacement.
Progressive weight-bearing advancement requires careful monitoring of healing progress through clinical examination and radiographic assessment. Most patients transition to full weight-bearing between 6-12 weeks post-operatively, though complex procedures such as Lapidus fusion may require extended protection periods. Physical therapy typically begins once adequate bone healing has occurred, focusing on range of motion restoration, strength training, and gait normalisation to achieve optimal functional outcomes.
Long-term success following bunion treatment depends heavily on patient compliance with footwear recommendations and lifestyle modifications that prevent recurrence of the underlying factors contributing to deformity development.
Footwear education remains crucial throughout the rehabilitation process, as inappropriate shoe selection represents one of the most common factors leading to treatment failure or deformity recurrence. Patients must understand the importance of maintaining adequate toe box width, avoiding excessive heel heights, and selecting shoes with appropriate arch support for their individual foot type. Custom orthotics may require periodic adjustment or replacement to maintain optimal biomechanical correction over time.
Long-term prognosis following bunion treatment varies based on multiple factors including deformity severity, treatment method selected, patient compliance, and individual healing characteristics. Conservative management typically provides sustained symptom relief in 60-80% of patients with mild to moderate deformities, though progressive worsening may occur in cases where underlying biomechanical factors remain unaddressed. Regular monitoring allows early intervention if symptoms worsen or deformity progression occurs.
Surgical outcomes demonstrate excellent long-term satisfaction rates exceeding 90% for appropriately selected cases, with most patients experiencing sustained pain relief and improved function for many years following surgery. However, potential complications including recurrence, overcorrection, or adjacent toe problems may develop in 5-15% of cases depending on the specific procedure performed and patient factors. Understanding these risks helps patients make informed decisions regarding treatment options.
Factors influencing long-term prognosis include patient age at treatment, underlying medical conditions affecting bone healing, activity level expectations, and compliance with post-treatment recommendations. Younger patients with isolated bunion deformity typically achieve better long-term outcomes compared to elderly individuals with multiple medical conditions or complex foot deformities requiring concurrent treatment. Realistic expectation setting proves essential for achieving high patient satisfaction rates regardless of treatment method selected.
Prevention of recurrent deformity requires ongoing attention to the factors that contributed to initial bunion development. This includes maintaining appropriate body weight, selecting proper footwear, addressing any underlying biomechanical abnormalities with orthotics or exercises, and monitoring for early signs of deformity progression. Regular podiatric follow-up allows early intervention if problems develop, potentially preventing the need for additional surgical procedures.
Quality of life improvements following successful bunion treatment typically include reduced pain levels, enhanced mobility, improved ability to participate in desired activities, and increased satisfaction with foot appearance. These benefits often extend beyond the immediate foot symptoms to include improved overall physical activity levels and enhanced psychological well-being. Patients frequently report increased confidence in social situations and reduced anxiety regarding foot-related limitations on their lifestyle choices.